I write in response to Prof David Cameron (Letters, 28 July). I also trained as a doctor during the 80s and early 90s and experienced the long working hours of that time. It is easy to fall into the trap of nostalgia and selective memory as we become older and detached from the frontline. I was looked after by the hospitals in which I worked, which were less managed than they are today. I worked in a close team, led by a consultant to whom I was responsible, and who was responsible for me. I spoke to no managers. I was provided accommodation, hot food day and night, and other privileges.
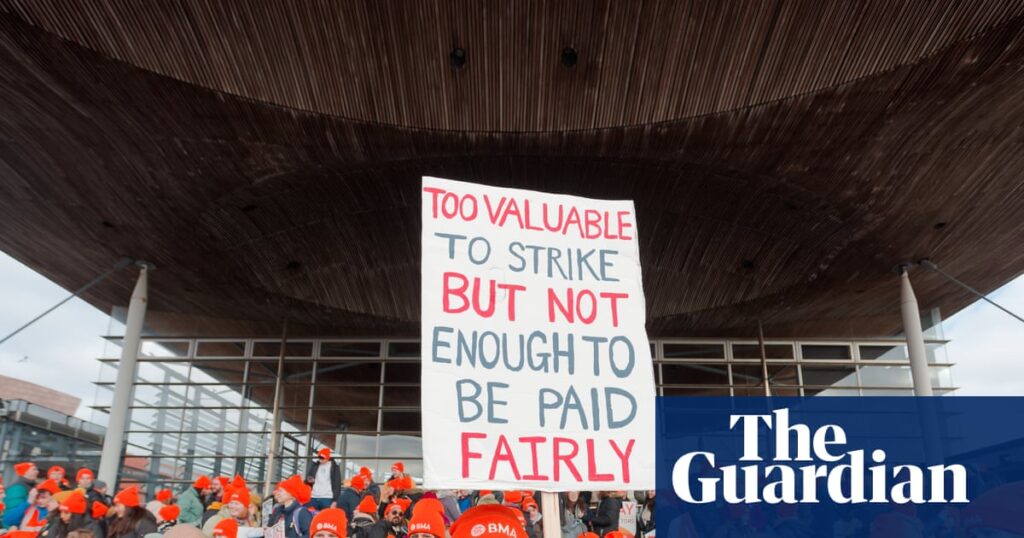
I speak to many young doctors in my current workplace and see the conditions in which they work. They are isolated and harassed by managers, who are in turn harassed by a target-driven culture. Their training is politicised and diluted by the physician assistant programme. They cannot get hot food after 4pm or at weekends, they pay for parking, they are ripped off by hospital accommodation services and see their pay eroded by below-inflation awards over many years. Small wonder they are angry. Pay is the quickest way by which they can obtain some redress for the deterioration in working conditions which they have suffered.
Dr Robin Hollands
Consultant, Shrewsbury
As a foundation year 1 (FY1) doctor who has nearly completed my first year of medical training, I have been deeply disheartened by the discourse around the resident doctor strikes. The British Medical Association (BMA) has failed to properly advocate for changes that will improve the working lives of doctors and the media has unsurprisingly been intensely critical of the BMA’s current objectives. It was exceptionally generous for the government to provide us with a 22% pay rise last year, but the BMA’s current demands for a further 29% are totally unrealistic and appear tone deaf to the many other public sector workers who have received much less. It is therefore not surprising that many media outlets have agreed that we are “greedy”.
Despite this, I believe the strikes are a representation of a much deeper dissatisfaction with the current state of affairs for resident doctors and this needs to be addressed. Resident doctors across the country are often working extensive hours on understaffed, dysfunctional hospital wards, with now ever-diminishing prospects of career progression. The latest BMA figures that 52% of FY2 doctors have no secure employment from August is deeply shocking and is a failure of the system that may threaten the future of the NHS.
It is time that both the BMA and the government woke up to the reality that there will be a severe doctor unemployment crisis unless urgent action is taken. This is the real problem that needs to be addressed. Pay restoration should absolutely remain a long-term goal, but there is little point improving my current resident doctor salary if there are no future pathways for resident doctors in the NHS.
Dr Will Giffin
Sheffield