When the air ambulance brought Jim Ashworth-Beaumont to King’s College hospital in south-east London, nobody thought he had a hope. He had been cycling home when a lorry driver failed to spot him alongside his trailer while turning left after a set of traffic lights. The vehicle’s wheels opened his torso like a sardine tin, puncturing his lungs and splitting his liver in two. They also tore off his right arm. Weeks after the accident, in July 2020, Ashworth-Beaumont would see a photo of the severed limb taken by a doctor while it lay beside him in hospital. He had asked to see the picture and says it helped him come to terms with his loss. “My hand didn’t look too bad,” he says. “It was as if it was waving goodbye to me.”
Ashworth-Beaumont, a super-fit and sunny former Royal Marine from Edinburgh, would go on to spend six weeks in an induced coma as surgeons raced to repair his crushed body. But as he lay on the road, waiting for the paramedics, his only thoughts were that he was dying. He did not have the wherewithal to consider the irony of his predicament.
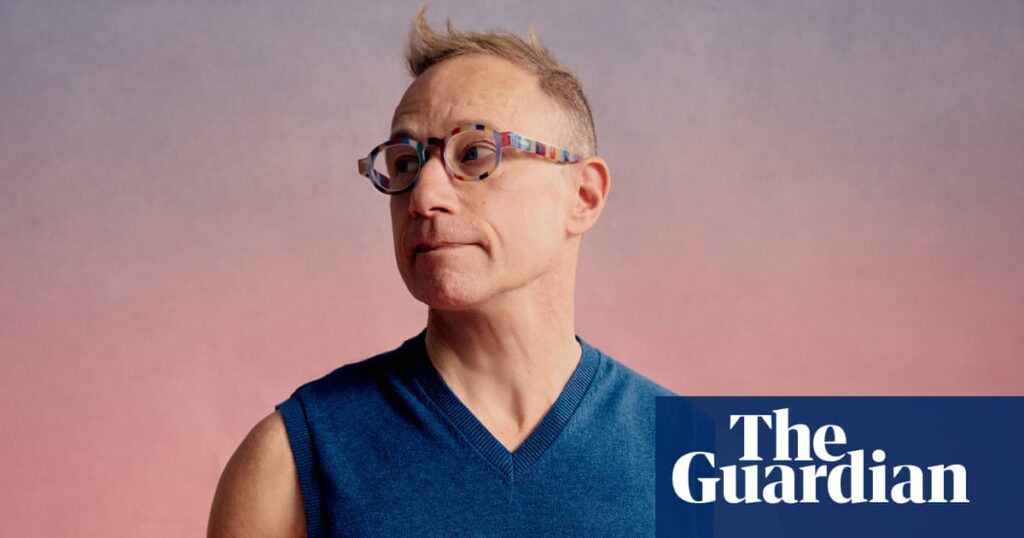
In the late 1990s, after he had left the marines, Ashworth-Beaumont, now 59, studied for a degree in prosthetics and orthotics at the University of Strathclyde in Glasgow. Clinicians in these disciplines help patients with pain, function and mobility by making and fitting devices such as prosthetic limbs and orthotic braces. He had written research papers and trained prosthetists while specialising as an orthotist at the Royal National Orthopaedic hospital (RNOH) in north-west London. “Now I was the patient,” he says.
I meet Ashworth-Beaumont for the first time in Greenwich Park, near the south London home he shares with his wife, Keri, a solicitor he met on a night out in 2002. It’s early summer 2024, almost four years after the accident in nearby Catford. He speaks softly through a smile that cracks only when he considers how far he has come and the support he has had: “Without Keri, I think I would have sat in a corner and wasted away.”
At first, his missing arm was a low priority for Edmund Fitzgerald O’Connor, the plastic surgeon who attended to his horrific abdominal injuries. But, by another twist of fate, the ambitious surgeon, who is 47, had a particular interest in limb loss. For years, he had been searching for the perfect candidate for a radical procedure he wanted to begin offering to amputees.
Osseointegration (OI), or direct skeletal fixation, is a relatively new way to attach prosthetic limbs. Rather than rely on a socket moulded to fit over a residual limb or stump – a method that dates back centuries – arms or legs are attached to a titanium implant inserted into the surviving bone (“osseo” means bone). Fixing a prosthesis to the implant, which emerges from the stump like a little tusk, is as easy as changing a camera lens.
OI patients need no longer tolerate irritation or infection where the socket rubs against skin and flesh. They gain a fuller range of motion and improved control and proprioception – the innate sense of where we and our extremities are in space. A prosthesis becomes part of the body rather than an awkward appendage. “It feels like I’ve got my own leg back,” Hanneke Mooij, a Dutch secretary, tells me three years after receiving an implant following decades of torment from ill-fitting sockets.
At the same time, rapid advances in electronic limbs mean surgeons can now effectively wire them into the brain. Taken together, OI and the latest prosthetics appear to bring a bionic future within reach. But the technique’s evolution has also been fraught, limiting its adoption. In a small number of cases, implants or bones have cracked. Painful infections have taken hold in the fleshy hole that surgeons must create around the implant. OI is also very expensive at a time when amputees struggle to access basic prosthetics care.
Fitzgerald O’Connor is convinced more of the 25,000 patients seen by the NHS prosthetics service each year could benefit from OI. When we first meet, the National Institute for Health and Care Excellence (Nice), the body that issues guidance on NHS treatment and funding, is reviewing OI. “When you’re doing 15 to 20 amputations a year and you have patients coming back with recurrent problems with their stump, it’s saddening to know there’s a viable alternative they can’t access,” he says.
The surgeon had been building a team to start offering OI, in the private sector at first, when he got the call from King’s. He had been searching for a patient who was resilient and in good health, who could help drive wider acceptance of the technique. If Ashworth-Beaumont could fund his treatment, his professional knowledge of what it takes to come back from a traumatic amputation would be a bonus. “You couldn’t have made up a better candidate,” Fitzgerald O’Connor says. “The conversation started in my mind the day he came in, but I wasn’t going to bring it to him until I knew he would survive.”
Osseointegration relies on a process that was discovered by accident. In the 1950s, Per-Ingvar Brånemark, a Swedish scientist based in Gothenburg, put optical devices housed in titanium into the legs of rabbits to observe the way bones heal. Once the study was over, the metal had fused to the bone and couldn’t be removed, defying conventional wisdom about the body’s tendency to reject foreign objects.
The discovery inspired Brånemark, who died in 2014, to invent dental implants, first used in the 1980s, that fuse to the jaw with titanium screws, removing the need for dentures. Wondering if the bond could hold larger devices, Brånemark and his son, Rickard, an engineer training as an orthopaedic surgeon, designed a larger implant. In 1990, they screwed two into the above-knee stumps of a woman who had been run over by a tram.
The procedure was eye-catching, evoking scenes from science fiction – Star Wars or The Six Million Dollar Man. It was also divisive. “I remember lecturing in the US in the late 90s when this senior professor stood up and said, ‘Only an idiot can believe this will ever work,’” says Rickard Brånemark, 65, who founded Integrum, the first OI company, in 1998. But a handful of enterprising surgeons saw an irresistible logic in bone-anchored prosthetics. Integrum soon had competition.
In Sydney, Australia, Munjed Al Muderis, an Iraqi-born orthopaedic surgeon who had fled Saddam Hussein’s regime after refusing to cut off the ears of draft dodgers, developed his own device, which he first implanted in 2008. He says patients have received more than 2,000 of his implants, which are hammered rather than screwed into bone. (Brånemark says surgeons have installed more than 700 Integrum devices.)
Al Muderis, 52, is the technique’s most bullish advocate. He is now offering it to victims of vascular conditions including diabetes, the biggest cause of leg amputations. (Other surgeons typically turn down such candidates, fearing their rehabilitation could be hampered by lifestyle factors.) “There is a big opportunity for this technology to take over from the traditional socket-mounted prosthesis,” Al Muderis insists via Zoom as he changes out of his scrubs.
The surgeon tells me about a current case he says demonstrates OI’s potential – a seven-year-old Iraqi orphan who lost an arm in a roadside dog attack while he slept. He was later adopted by a wealthy Chinese family. In the coming months, Al Muderis plans to fit the boy with an implant, which will need to be replaced as he grows. Unlike other OI surgeons, he argues that children can be suitable candidates despite the need for further operations. In the case of leg amputees, he says, OI gets children walking again sooner. “It’s all a balance,” he adds, pointing out that sockets in children need changing a lot more often than OI implants.
The boy will also undergo a procedure called targeted muscle reinnervation (TMR), which involves rerouting amputated nerves. This can help relieve pain in the stump, where the severed nerves can thicken into tumour-like neuromas. Remarkably, it can also help amputees control prosthetic limbs with their minds.
To achieve this, Al Muderis will surgically attach the severed nerves, which had travelled to muscles in the boy’s arm and hand, to small, inessential sections of muscle in his chest instead. Tiny electrodes implanted under the skin will connect these muscle sites to the prosthetic arm via eight cables wired through the body and the titanium implant. When the boy moves to grab a water bottle, his brain will activate the chest muscles, which will forward the signal to the corresponding motors in his arm and hand. “It’s amazing because the transmission is instant,” Al Muderis says of TMR, which he adds is not yet widely available.
Integrum has also adapted its implants to allow amputees to upgrade to TMR and other advanced control systems in the future. Yet Al Muderis – who, like Brånemark, has been to Ukraine to offer OI to injured soldiers – says scepticism holds back the technique, including in the UK. He partly blames regulations and resistance to the idea of an implant that perforates the skin: “This is a completely revolutionary technology which violates many of the principles of orthopaedics.”
Brånemark is more conservative but also thinks far more amputees could benefit than the few thousand globally who have implants. When Fitzgerald O’Connor told him about his plans and the unlikely case of the one-armed prosthetist, the Swedish surgeon agreed to back his British OI team and oversee its first operation. “A lot of people still don’t know about OI, even in Sweden,” Brånemark says. “As someone who also works in the field, Ashworth-Beaumont can be a really good advocate.”
For weeks, HIs life hung in the balance. He had lost almost all liver and kidney function. Sepsis set in as he lay in a coma. His first wife and their two grown-up children came down from Scotland to say goodbye. “The first thing I remember, coming out of the coma, was my daughter’s face; it’s still a really strong image in my mind,” Ashworth-Beaumont says. He thinks he inherited his fighting spirit from his father, a docker’s son from Liverpool, who worked as a bellboy before becoming a successful restaurateur. His mother still runs a gift shop in her 80s. He also has childhood memories of a cousin who lost his legs in a car crash. “I guess amputation was always on my radar,” he says.
After struggling to focus at school, at 16 he joined the marines, where he excelled. Fitness was a passion, and he became skilled in mechanical and electronic engineering, which led to his prosthetics career. In the final year of his degree, begun in 1996, he worked at Steeper, a British prosthetics firm that would one day supply his motorised elbow. He joined the RNOH in 2005 while racing in triathlons and moonlighting as a personal trainer. He was at peak fitness when the lorry hit him.
after newsletter promotion
While amazed to be alive, Ashworth-Beaumont realised his limitations as soon as he tried to shift his weight around in his hospital bed. “I knew these things professionally, but it really brings it home when you first try to move your shoulder and nothing happens.” As his vital organs rallied, he became determined to return to work. He would need a highly functional prosthesis; his job is physical, requiring the manipulation of limbs, as well as the making and fitting of devices. He was all ears when Fitzgerald O’Connor shared his plans. He also knew it would take time, and that the advice in prosthetics care is to try standard devices first.
It was almost a year after his accident, when he was about to return to work, that Ashworth-Beaumont received a body-powered arm on the NHS. These mechanical devices are a step up from static prostheses, which can incorporate hooks or skin-coloured hands. By rounding his shoulders, he could open a metal claw attached by a cable to a back harness: “It works, but the technology has been around for hundreds of years.”
Socket attachments date back to the 16th century or earlier. Designs and materials have changed, but the principle is the same: a socket must grip the stump for good function but not so tightly as to cause discomfort. Suction helps keep a socket on, but Ashworth-Beaumont needed strapping to pull his against his short stump, which further limited comfort and mobility. He ended up wearing the arm for just a few hours a day at work, and describes a circular problem for arm amputees. The motivation to use a prosthetic leg is high, to avoid relying on crutches or a wheelchair: “But there’s so much we can still do with one arm.” Patients tend to get frustrated with prosthetic arms, often stashing them away and making do. Ashworth-Beaumont says this partly explains a reluctance in the NHS to offer advanced devices, particularly early on. “But the problem is they’re also not giving people the opportunity to try these components when so many of us would benefit.”
He went private to get a better arm sooner, using money raised from a legal settlement with the lorry company and a family crowdfunder. Working with Alan McDougall, a prosthetist at Proactive, a private clinic in Surrey, he upgraded to a stealthy black electric device with motors in the elbow, wrist and hand. He learned to flex his residual biceps and triceps independently to activate the motors, via sensors built into the socket. Subtle hand movements allowed him to adopt different grips. It’s a step below TMR, but it works: I see it in action when we next meet and Ashworth-Beaumont gives me one of the firmest handshakes I’ve had.
The electric arm, which is worth more than £100,000, meant he could do more, but it further exposed his socket’s shortcomings. It was heavier than the NHS device, requiring a tighter, less comfortable fit. He could pick up a mug, say, but the flesh interface also made it hard to position the hand precisely, creating a lag between brain and hand. OI increasingly felt like the solution. Ashworth-Beaumont considered himself an overqualified guinea pig with an opportunity to highlight his profession and widen access to the latest tech. “I see it almost as a duty to explore the possibilities,” he told me in 2021, when I first got in touch.
Ashworth-Beaumont would not be the first British amputee to receive an Integrum implant. Starting in the late 90s, Brånemark’s new devices were used in a trial involving 18 patients at Queen Mary’s hospital in Roehampton, south-west London, where the modern British prosthetics industry emerged after the first world war. While the trial had some success and provided valuable data, the experience of its least fortunate participants still reverberates around the field and the debate about NHS provision.
Gemma Trotter, a fitness instructor from south London, was 16 when she had a leg amputated above the knee after a car crash. Held back for years by uncomfortable sockets, she set aside her reservations about OI, which she had viewed as “crackers”, and joined the trial in 2003, aged 21. It was transformative. “Suddenly I could feel the floor through my leg again. If I wore jeans, a lot of people didn’t even know I was an amputee,” she says. “I got married, had a baby … they were the best nine years of my life.”
Then the implant broke and became infected. By then the trial team had disbanded, limiting follow-up care. Trotter, now 42, has endured more than a decade of pain and attempted fixes by surgeons including Brånemark. She is waiting to have her third implant removed after more problems, and won’t risk having another. (Brånemark tells me that, while there is a risk of failure with any implant, Integrum’s success rate has significantly improved since the Roehampton trial.)
Trotter remains one of only a few dozen patients in the UK who have had OI, which is more widely available in countries with insurance-based health systems. Hanneke Mooij, the Dutch patient, is surprised to hear OI is hard to access in the UK. She received an Integrum device in 2022, 36 years after losing her leg in a motorbike crash. She is part of a Dutch group of 20 one-legged female friends who call themselves “the flamingos”, half of whom have had OI surgery in the past few years. “I’m convinced this is the future,” she says.
Most British OI recipients are patients at Relimb, a private clinic founded at the Royal Free hospital in north-west London in 2018. Its directors, Norbert Kang and Alex Woollard, use Al Muderis’s implants and have about 60 patients on their books, almost all funded by legal settlements after traumatic accidents. Partly with the Roehampton trial in mind, they do not think the NHS has the resources to offer the skilled and long-term care required to make OI successful. “No matter how beneficial it is and how well we can do it now, we’re not going to change health economics,” Woollard says.
He and Kang are not alone in having doubts. Nicky Eddison, chair of the British Association of Prosthetists and Orthotists, says the professions are already facing a staffing and recruitment crisis, and some NHS trusts are making do with just two specialists. “Whatever technical advances you make, we can’t deliver them without skilled clinicians,” she says.
Yet proponents of OI make a case for long-term cost savings. Stephen Cruse, founder of the Amputation Foundation, a charity in Merseyside, had OI surgery with Al Muderis in 2016, eight years after losing his legs in a car crash while in Australia. After returning to the UK, he convinced an Australian government compensation scheme to fund his surgery after calculating it would save money in five years. “They were paying about £30,000 a year on sockets, liners and maintenance,” says Cruse, who had a “nightmare” with sockets but now rarely needs to see his prosthetist.
Last December, Nice published new guidelines. It now recommends that OI can be used in the NHS but only by multidisciplinary teams with specific training, and the NHS tells me its policy – not to offer it widely – isn’t changing, based on the risks and its funding priorities. Fitzgerald O’Connor says there may be ways to secure funds in exceptional cases, and he will continue to push for wider access as evidence of OI’s efficacy grows. “To leave it in a silo, where it’s only accessible with vast amounts of money, does a disservice to patients who are suffering,” he says.
After long delays caused by Covid and post-Brexit paperwork, Ashworth-Beaumont finally gets a date for his private surgery: a Saturday in October 2024. “I tend to take things in my stride, but it feels like jumping out of a plane,” he tells me a few weeks before the operation. “You know the systems are there to protect you, but there’s always that 1% chance things could go awry.”
The day before the surgery, which will take place at St Thomas’s hospital in central London, I join Ashworth-Beaumont at a private clinic farther up the Thames at Battersea power station. Fitzgerald O’Connor and Aaron Saini, an orthopaedic surgeon who is also part of the new OI team, have gathered amputees and professionals to discuss this case and prosthetics technology more widely. The subject of NHS care keeps cropping up.
Craig Mackinlay, a former Conservative MP from Kent, lost all four limbs to sepsis in 2023. Five months later, he received a standing ovation when he strode into the House of Commons wearing prostheses. Fitzgerald O’Connor, who performed the amputations, looked on from the public gallery. It was a triumphant comeback, but Mackinlay has since highlighted NHS shortcomings, including long waits and early black rubber prostheses that resembled “clubs … I couldn’t see what they’d be good for apart from breaking windows or pub fights.”
Mackinlay, now a life peer, has since gone private, with support from device firms and his own money. In a debate in the Lords this May, he said he would still be in a wheelchair had he not accessed better legs sooner. “The technology is out there and the NHS will give some of it to you, but it takes years,” he says. “Why are we holding people back?” In response, Baroness Merron, a health minister, announced a review of the provision of advanced prostheses. In a statement, an NHS spokesperson insists that it “provides a comprehensive package of care and support for people who have lost limbs, including a range of prosthetics”.
When I ask Ashworth-Beaumont if everything is starting to feel a bit real, he takes a deep breath. “This is all positive,” he says, his voice cracking. “Sorry, I’m just thinking about the last four years.” Fitzgerald O’Connor places a hand on his shoulder. “It was tough, but you made it,” he says. The next morning, Brånemark, Fitzgerald O’Connor and Saini screw the Integrum implant into Ashworth-Beaumont’s humerus, carefully rebuilding his soft tissue around it. “I’ve been walking around like I’m made of crystal,” he tells me two days later via Zoom as he waits for bone and metal to bond.
Not long after Christmas, he is ready for an arm. McDougall has adapted Ashworth-Beaumont’s body-powered device so he can attach it to his implant. Even with the encumbrance of the cable and harness needed to move the hand, he is struck by the enhanced control of a firmly anchored limb. “I went out for dinner with Keri for my birthday and used a knife and fork properly,” he says. “I feel more competent as an individual.”
By early March he is ready to go full bionic, connecting his heavier electric arm. At Proactive, plaster casts of stumps stand like sculptures in the workshop. As well as adapting the more advanced arm, McDougall has added a small cuff to house the muscle sensors that used to sit inside Ashworth-Beaumont’s socket. The arm would look at home in a sci-fi props department, with its carbon fibre-effect shell and translucent glove, which reveals some of the hand’s moving parts. Then there’s the gap in the upper arm, where only the titanium implant links flesh to hardware. Yet when the prosthesis hangs from Ashworth-Beaumont’s shoulder, it somehow looks like part of him. Without the socket and straps, his silhouette is symmetrical: he is whole again.
Soon motors whirr as he tests his bionic joints, raising his arm above his head in a way he hasn’t been able to do since the accident. McDougall adjusts it using a Bluetooth-connected iPad app. “This is really good,” Ashworth-Beaumont says as he picks up a stray screw from a workbench. Within days, he’s performing tasks previously beyond him. Hoovering feels like a privilege.
Five years after his old arm appeared to wave goodbye, Ashworth-Beaumont is as aware as anyone of the limitations of the health service. “I’ve spent, what, five hours with Alan today, there’s no way you’d get that time in the NHS,” he says. While he watches the OI debate continue, returning to his own NHS job has felt like his biggest achievement. As well as being able to meet the physical demands of his work, his ordeal has changed his relationship with patients. “I was quite emotional about it after my first few appointments,” he says. “I really did know how they felt.”